What Is Diabetic Retinopathy?
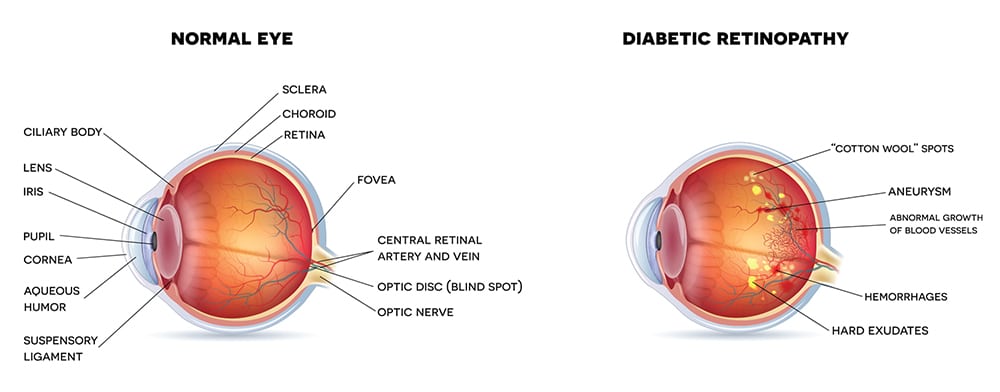
Diabetic retinopathy is a complication of diabetes that affects the eyes. The length of time a person has diabetes determines his or her likelihood of developing diabetic retinopathy. It is the most common diabetic eye complication, and a leading cause of blindness in American adults. Diabetic retinopathy causes the blood vessels that supply nourishment to the retina, the light-sensitive lining in the back of the eye where vision is focused, to weaken, swell and leak, causing a loss of vision.
What Are The Symptoms Of Diabetic Retinopathy?
In the early stages of diabetic retinopathy, patients usually do not show symptoms, and treatment is not always required. Patients have to monitor their blood-sugar levels to prevent the condition from worsening. If it does, prompt treatment is necessary to preserve vision.
Patients who develop diabetic retinopathy may not, at first, notice any changes to their vision. In its earliest stages, the condition causes tiny areas of swelling in the small blood vessels of the retina. Once symptoms are present, they include the following:
- Blurred or double vision
- Seeing flashing lights, blank spots or dark floaters
- Pain or pressure in either or both eyes
- Problems with peripheral vision
In its advanced stages, diabetic retinopathy can cause irreversible blindness.
During any stage of diabetic retinopathy, a condition known as macular edema can develop. Macular edema is the buildup of fluid in the macula, the light-sensitive part of the retina that allows objects to be seen with great detail. As the macula swells, vision becomes blurred. About half of the people with proliferative retinopathy (the most advanced stage) are diagnosed with macular edema.
Stages Of Diabetic Retinopathy
Diabetic retinopathy has four stages, each one increasingly serious:
- Mild nonproliferative retinopathy
- Moderate nonproliferative retinopathy
- Severe nonproliferative retinopathy
- Proliferative retinopathy
As the disorder worsens, more and more blood vessels are affected. By the time a patient has proliferative retinopathy, the body is creating new blood vessels to replace the ones that are blocked. The problem is that the new blood vessels have very thin walls. If they leak blood, severe vision loss or blindness can result.
How Is Diabetic Retinopathy Diagnosed?
Diagnosis of diabetic retinopathy requires a thorough eye examination that includes the following:
- Visual-acuity test
- Dilated-eye examination
- Tonometry test
- Retinal exam
- Fluorescein angiogram
Prior to some of these tests, eye drops containing a stain are administered so that the doctor can see the blood vessels more clearly.
Diabetic Retinopathy Treatment Options
Other than controlling blood pressure, blood cholesterol and blood sugar, treatment is not needed during the first three stages of diabetic retinopathy. The fourth stage, proliferative retinopathy, is treated with a laser surgery known as scatter laser treatment. During the procedure, the abnormal blood vessels are ablated, causing them to shrink.

This procedure works best once the blood vessels begin to bleed. Severe blood-vessel bleeding may need to be surgically corrected with a vitrectomy, during which blood is removed from the eye.
Treatment for macular edema usually includes a laser procedure called focal laser treatment. During this procedure, several hundred small laser burns are made in the areas of retinal leakage to reduce the amount of fluid in the retina. This helps reduce the risk of vision loss, and may improve lost vision in a small number of cases. Focal laser treatment is performed in a doctor’s office, and can usually be completed in just one session.
Risk Factors Of Diabetic Retinopathy
A patient with diabetes should have an annual comprehensive dilated-eye exam. In the United States, more than 40 percent of diabetics have some form of diabetic retinopathy.
The risks of developing diabetic retinopathy can be minimized by doing the following:
- Monitoring changes in vision
- Keeping blood-glucose levels low
- Monitoring and managing blood pressure
- Eating a healthy diet
- Participating in a regular exercise routine
- Monitoring and managing cholesterol levels
Patients with proliferative retinopathy can reduce their risk of blindness by 95 percent by keeping up with medical examinations, and promptly getting necessary treatment.
Diabetic Retinopathy FAQs
Q: What Is Diabetic Retinopathy?
A: Diabetic Retinopathy is changes to the retina due to diabetes. It commonly appears in people that do not manage diabetes properly. It needs to be monitored and possibly treated regularly.
Q: What Are The Causes Of Diabetic Retinopathy?
A: Diabetic Retinopathy results from the damage diabetes causes to the small blood vessels in the retina. The damaged vessels can cause vision loss.
Q: What Happens If It Is Not Treated?
A: If Diabetic Retinopathy is not treated, one can potentially go blind.
Have questions about Diabetic Retinopathy?
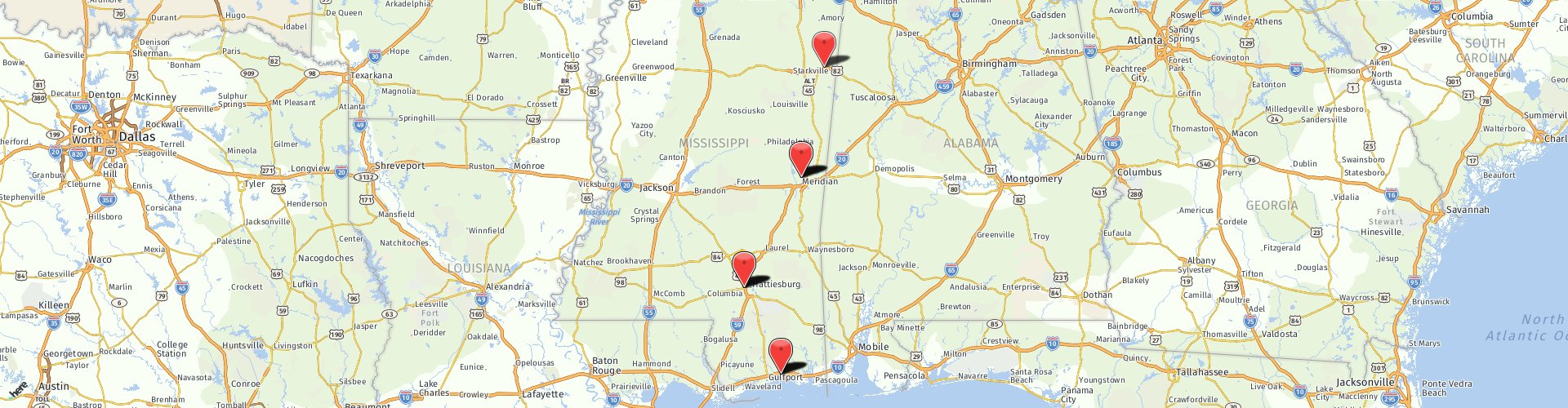
If you have questions or need more information about Diabetic Retinopathy, please feel free to contact the Retina Specialists of Mississippi at 601.255.0736 or fill out the contact form by clicking here.